Blog
How Osteoarthritis Can Affect the Ankle

Osteoarthritis, or OA, which is often associated with aging and wear-and-tear, isn't limited to just the knees and hips. It can also affect the ankle joint, causing pain and mobility issues. Osteoarthritis in the ankle is a chronic condition that develops when the protective cartilage that cushions the bones begins to deteriorate. OA can occur at any time of life, but it is most common in older adults. Being overweight adds stress to your ankles and fat cells produce proteins that may make the condition worse. Any ankle injury, even one that happened years ago, can lead to osteoarthritis. Symptoms include pain, stiffness, swelling, and a reduced range of motion, which can significantly affect your daily life. Even simple tasks like walking and climbing stairs can become challenging. Several factors can contribute to ankle osteoarthritis, including previous injuries, genetics, and obesity. Treatment options include medication, physical therapy, orthotic devices, and in some cases, surgery. Osteoarthritis is a progressive disease, and for that reason managing it requires a comprehensive approach to reduce pain and maintain mobility. It's suggested that you make an appointment with a podiatrist if you suspect osteoarthritis is affecting your ankles.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Pennsylvania. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Diabetic Foot Ulcers
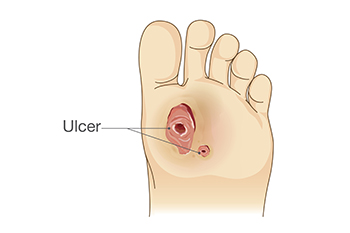
A foot ulcer is defined as any break in the skin. It is the most common type of diabetic foot wound and can lead to loss of functioning and severe complications. These foot wounds often result from factors such as poor blood sugar control, diabetic peripheral neuropathy, and abnormal foot mechanics due to deformities. Diabetic peripheral neuropathy, a side effect of diabetes, can also lead to a loss of protective sensation in the feet, making early injury detection challenging. The assessment of the diabetic foot involves a comprehensive foot and body examination. This can consist of assessing risk factors, undergoing a dermatologic and musculoskeletal evaluation, and having neurologic tests that can determine the degree of sensation. Treatment of diabetic foot ulcers includes debridement, wound culturing, and wound dressings. Additionally, it is important to monitor glycemic control and infection control. Their prevention and management are essential to improve the patient’s quality of life. If you have diabetes and have developed a foot wound or any other foot condition, it is strongly suggested that you make an appointment with a podiatrist who can evaluate your situation, and receive the appropriate treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Pennsylvania. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes and Symptoms of Bunions

A bunion is a common foot deformity that affects the joint at the base of the big toe. This condition occurs when the big toe deviates outward, causing the joint to protrude and creating a visible bump on the side of the foot. Bunions typically develop over time due to a variety of factors. Genetics plays a significant role, as the shape and structure of your foot can predispose you to bunions. Wearing ill-fitting shoes, especially those with narrow-toe boxes or high heels, can exacerbate the condition. Additionally, inflammatory joint conditions like arthritis may contribute to bunion formation. The symptoms of a bunion can range from mild to severe. Common signs include pain, swelling, redness, and tenderness around the affected joint. Over time, the big toe may angle towards the other toes, causing discomfort and difficulty finding well-fitting shoes. The skin over the bunion may become thickened and calloused. For some individuals, bunions can restrict their daily activities and lead to further foot problems if left untreated. If you have developed a bunion, it is strongly suggested that you consult a podiatrist who can offer you relief and treatment options that are right for you.
If you are suffering from bunion pain, contact one of our podiatrists of Pennsylvania. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.

